Beyond the Buzzword: What Real AI Looks Like in Clinical Research
Every company seems to claim they’re “using AI.” Yet if you ask how, the answers often fall apart under scrutiny. In clinical research, the difference between buzzword AI and real AI is more than semantics. It determines whether technology accelerates discovery or just adds noise.
Why “AI” Became a Catch-All
Artificial intelligence has become one of the most overused terms in healthcare. A system might run a simple keyword search or apply basic rules to structured data and still be labeled “AI-powered.” That’s a problem. Because in medicine, language isn’t simple, and context can’t be guessed.
Clinical data lives in two worlds: structured information like labs and diagnoses, and unstructured text like physician notes, pathology reports, and discharge summaries. According to recent research published in the National Library of Medicine’s database, up to 80% of clinically relevant data in EHRs is unstructured data often overlooked by conventional systems.
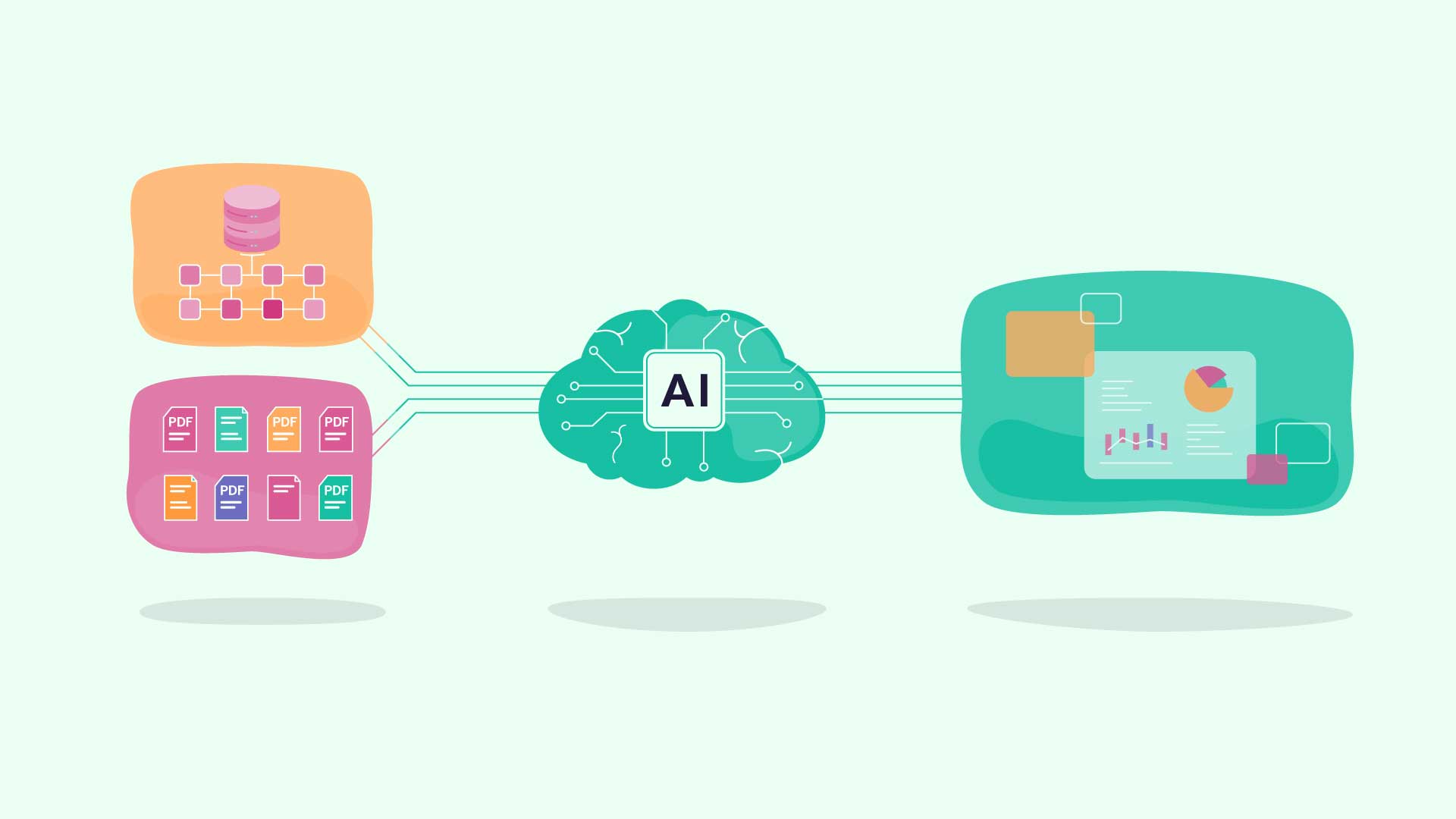
The Anatomy of Real AI
Real AI doesn’t just process data, it understands it. In research, that means models trained on medical ontologies, natural language processing tuned to clinical language, and feedback loops that constantly refine accuracy.
True AI systems can:
-
Recognize synonyms, abbreviations, and shorthand (e.g., “NASH” vs. “fatty liver”).
-
Infer context and temporal relationships (e.g., “history of diabetes” vs. “currently diabetic”).
-
Learn continuously as more real-world data enters the network.
These are the capabilities that help AI bridge what researchers call the data-to-evidence gap—turning raw EHR inputs into structured insights that can actually guide research
Marketing AI vs. Meaningful AI
There’s a difference between marketing AI and meaningful AI. Marketing AI automates headlines: it looks good on a slide but stops at simple pattern recognition. Meaningful AI automates hard work: it reads unstructured data, interprets clinical nuance, and generates evidence that holds up to scientific scrutiny.
Meaningful AI is transparent, auditable, and built to work alongside people, not instead of them.
That last point matters. As the Brookings Institution highlights in its analysis on human factors shaping AI’s impact in health care, the most effective AI is human-centered. It’s built to augment, not replace, clinical judgment. The best systems make professionals more capable, not redundant.
Humans in the Loop By Design
In clinical research, trust comes from validation. That’s why the most advanced AI platforms use a human-in-the-loop approach, where algorithms identify potential patients or data points and clinical experts confirm accuracy.
This hybrid model ensures that automation handles scale, while human expertise ensures precision. It’s not about eliminating jobs, it’s about eliminating inefficiency. Site coordinators, nurses, and data specialists can spend less time buried in charts and more time engaging with patients, improving study design, or expanding research capacity.
From Hype to Human Impact
When you cut through the hype, the question isn’t whether AI belongs in clinical research—it’s how it’s used.
- Is it helping researchers make faster, more accurate decisions?
- Is it connecting more patients to trials they qualify for?
- Is it generating trustworthy evidence that reflects real-world populations?
Real AI answers “yes” to all three. The future of clinical research won’t be run by algorithms alone. It will be powered by scientists, coordinators, and clinicians working with technology that finally understands the data they’ve been struggling to use for decades.
These principles define how we built BEKplatform. Its ontology-driven AI interprets both structured and unstructured clinical data, while our human-in-the-loop model ensures every match is contextually sound. Unlike tools limited to billing codes or keywords, BEKplatform understands the way clinicians actually write and think, capturing medical nuance, abbreviations, and context from narrative notes to reveal insights hidden in plain text.
Not all AI is created equal. In clinical research, the difference comes down to the understanding of data, medicine, and the people behind both. The systems that learn that difference will be the ones that truly move science forward.
Read More
Why “Eligible Patients” Aren’t Always Enrollable Patients
Why “Eligible Patients” Aren’t Always Enrollable PatientsThe industry’s reliance on eligibility as a proxy for enrollment is understandable. Protocols are built around eligibility criteria. Feasibility assessments often rely on structured EHR data and historical...
Why Traditional Feasibility Fails (and What Actually Predicts Enrollment Success)
Why Traditional Feasibility Fails (and What Actually Predicts Enrollment Success)Clinical trial feasibility is intended to answer a straightforward question: Can this study realistically enroll patients?Yet across therapeutic areas and trial phases, studies that pass...
American Hospital Association: How AI Is Transforming Clinical Trials
Top AI-Driven Clinical Trial Patient Identification Tools: What Research Teams Should Look for in 2026
Top AI-Driven Clinical Trial Patient Identification Tools: What Research Teams Should Look for in 2026Clinical trial enrollment remains one of the most persistent barriers in research. Even when the right patients exist within a health system, identifying them often...